Epiretinal Membranes
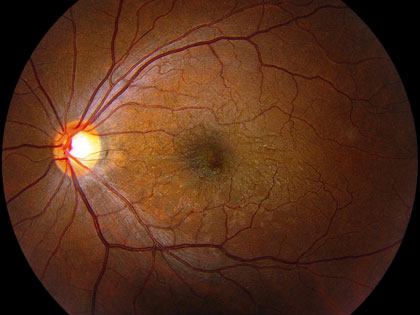 Epiretinal Membranes, or Macular Puckers: A very fine cellophane-like membrane may occasionally form over the surface of the macula, the central portion of the retina. These membranes may form as the result of a previous tear or detachment of the retina, or other retinal diseases, but many times they are idiopathic, meaning their cause is unknown. Often, the membrane may be so thin and fine as to be completely asymptomatic, and it may be diagnosed during a routine dilated eye exam. In these cases, no treatment will be necessary, although periodic follow-up exams may be recommended. Occasionally, however, the membrane may slowly grow and thicken over time, causing wrinkling and swelling of the underlying macula and distortion and blurring of the vision. This is sometimes referred to as a macular pucker. When this occurs, surgery may be required to peel the membrane from the surface of the macula in order to allow it to smoothen out. This is usually done in conjunction with removal of the gel from within the eye, a procedure called vitrectomy. Vitrectomy with membrane peeling is performed in an operating room, usually as an outpatient procedure. Postoperatively, there is usually little or no discomfort and minimal restriction on activity. However, it can take up to a few months for the vision to improve significantly and it may never recover to the point where it was prior to the formation of the membrane. Risks of the surgery are the same as with vitrectomy for any other problem, namely a significant risk of cataract development, usually within two years, but often sooner, and a lower but not insignificant risk of retinal detachment. Both of these problems can be addressed with additional surgery if necessary, but these risks always remain a consideration when thinking about vitrectomy surgery.
Epiretinal Membranes, or Macular Puckers: A very fine cellophane-like membrane may occasionally form over the surface of the macula, the central portion of the retina. These membranes may form as the result of a previous tear or detachment of the retina, or other retinal diseases, but many times they are idiopathic, meaning their cause is unknown. Often, the membrane may be so thin and fine as to be completely asymptomatic, and it may be diagnosed during a routine dilated eye exam. In these cases, no treatment will be necessary, although periodic follow-up exams may be recommended. Occasionally, however, the membrane may slowly grow and thicken over time, causing wrinkling and swelling of the underlying macula and distortion and blurring of the vision. This is sometimes referred to as a macular pucker. When this occurs, surgery may be required to peel the membrane from the surface of the macula in order to allow it to smoothen out. This is usually done in conjunction with removal of the gel from within the eye, a procedure called vitrectomy. Vitrectomy with membrane peeling is performed in an operating room, usually as an outpatient procedure. Postoperatively, there is usually little or no discomfort and minimal restriction on activity. However, it can take up to a few months for the vision to improve significantly and it may never recover to the point where it was prior to the formation of the membrane. Risks of the surgery are the same as with vitrectomy for any other problem, namely a significant risk of cataract development, usually within two years, but often sooner, and a lower but not insignificant risk of retinal detachment. Both of these problems can be addressed with additional surgery if necessary, but these risks always remain a consideration when thinking about vitrectomy surgery.
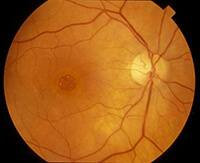
Macular Holes: The center of the retina is called the macula, and the very center of the macula is called the fovea. It is this central portion of the macula that is responsible for our very finest detailed central vision. Interestingly, the foveal portion of the macula is also the very thinnest part, making it susceptible to the formation of a hole. This is usually a spontaneous painless occurrence, more common in people in their fifties and sixties, but rarely it can be the result of trauma as well. The hole begins as a small partial defect, which may result in a mildly blurred or distorted central vision. If it progresses to a larger full-thickness hole, the central vision may be lost entirely. Even in these cases, the more peripheral portion of the vision is never affected and the eye retains useful vision, but not the ability to read. In a significant portion of cases, a partial thickness small hole will resolve and heal on its own without treatment. In these cases, observation alone may be the best plan. Once a larger full-thickness hole has developed, however, surgery will be required to close it. The timing of the surgery is usually not critical, but results seem to be better if it is performed within about a year of the hole formation. As in epiretinal membranes in the above section, vitrectomy surgery will be performed, but, in this case, the eye will also be filled with a bubble of gas. The patient will then be required to keep their face down so that the bubble can float up against the hole in the back of the eye and seal it closed. The gas bubble may last several weeks in the eye, and the patient may not fly in an airplane until it has disappeared. The patient will not be required to keep the face-down position for this entire time, but the exact number of days is somewhat controversial as of this writing in 2009. It may range anywhere from one or two days up to two weeks or more, depending on the surgeon and the case. During this period, the patient will be encouraged to maintain strict face-down position both day and night. Special cushions and chairs may be available to help the patient do this more comfortably. Approximately 90% of macular holes can be closed with one surgery, and most of the remaining 10% can be closed with a second. If the hole is closed successfully, most, but not all, patients experience a substantial improvement in their vision, although there is almost always some degree of residual blurriness or distortion which is permanent.